Acute upper respiratory tract infections (URTIs) remain one of the most common reasons for patient consultations in both primary care and integrative health settings. Though often self-limiting, URTIs are frequently treated with antibiotics, despite strong evidence that most cases are viral in origin and would resolve without such intervention. The resulting over-prescription contributes directly to the global crisis of antimicrobial resistance, a challenge that demands new strategies rooted in both effectiveness and sustainability.
For homeopaths, this is familiar territory. Homeopathy has long offered a patient centred, non-invasive approach to managing acute respiratory infections. In many parts of the world, France, Germany, India, Brazil, to name just a few, it is already widely used for this very purpose. Patients and practitioners alike have seen its capacity to reduce symptom severity, shorten illness duration, and support long-term immune resilience. Still, it is always encouraging to see such clinical experience reflected and validated in peer reviewed scientific literature. A recently published real world cohort study by Banik et al., appearing in the peer‑reviewed journal Complementary Medicine Research (January 2025), delivers precisely that recognition.
This real world cohort study examined outcomes for 18,850 patients presenting with acute URTIs to either homeopathic or conventional general practitioners in Germany. It tracked their recurrence rates and antibiotic prescriptions over the following 12 months. The study’s observational design, based on actual clinical practice rather than experimental settings, makes its conclusions highly relevant to practitioners on the ground.
Patients were grouped according to the type of care they received. Those in the homeopathy group were treated primarily with individualised or complex homeopathic remedies, while those in the conventional group received standard pharmacological treatment; typically involving antipyretics, analgesics, and, in many cases, antibiotics. What emerged was a striking difference in both the recurrence of infections and the use of antibiotics.
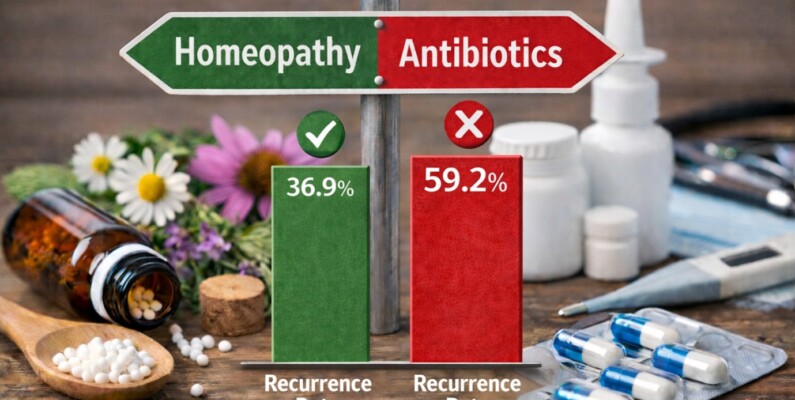
In the homeopathy group, only 36.9% of patients experienced a recurrence of URTI symptoms within the follow up period, compared to 47.6% in the conventional care group. This difference, which remained statistically significant after adjusting for demographic and clinical variables, points to a key strength of homeopathy; its ability not only to resolve acute symptoms but also to strengthen the individual’s susceptibility over time. For homeopaths, this aligns closely with the principles we uphold; that well-chosen remedies can stimulate the body’s own healing responses, improving health beyond the acute episode.
Homeopathy v Antibiotics
Perhaps even more noteworthy was the dramatic difference in antibiotic use. In the homeopathy group, only 20.7% of patients were prescribed antibiotics, compared to 59.2% in the conventional treatment group. In other words, patients under homeopathic care were three times less likely to receive an antibiotic. Given the global urgency around antibiotic resistance, this is more than just an academic finding, it’s a public health imperative. Homeopathy presents a proven, scalable way to reduce antibiotic overuse, especially in cases where the drugs offer no therapeutic benefit.
Importantly, the study found no indication that this reduction in antibiotics compromised patient outcomes. There was no increase in complications, dissatisfaction, or need for follow up interventions in the homeopathy group. On the contrary, these patients not only had fewer recurrences but also experienced a course of treatment that aligned with the body’s natural processes. It is a potent reminder that less can indeed be more when clinical judgment and patient centred care guide decision making.
Data driven support for what we already observe in practice
For homeopaths and students alike, the study provides both affirmation and opportunity. It offers data driven support for what we already observe in practice, and it gives us a tool to communicate the value of homeopathy to colleagues, patients, and policymakers. When patients are unsure about non-pharmacological approaches or when conventional practitioners raise concerns about efficacy, having such real world evidence at hand can be invaluable.
It also reflects a broader trend in healthcare; the shift toward real world evidence (RWE) as a complement to the more traditional randomised controlled trials. While RCTs remain the gold standard for many regulatory purposes, RWE is increasingly recognised for its ability to capture the nuances of daily practice and complex patient interactions. This trend aligns well with the philosophy of homeopathy, which emphasises individualised care and outcome based practice rather than one-size-fits-all protocols.
Information Exchange: Dr Varsha Khurana’s clinical experience managing acute coughs
To further this mission, HINT hosts monthly Information Exchange Events, providing a regular platform for practitioners, researchers, and students to share insights, examine current evidence, and engage in meaningful discussion on clinical practice. These sessions offer an invaluable opportunity to deepen professional understanding and remain connected to developments in homeopathic healthcare. At a recent event, Dr V. presented a compelling account of her clinical experience in managing acute coughs, highlighting practical strategies and remedy choices that resonated with many in attendance. These events are not only a rich source of continuing professional development but also a way to stay actively involved in the evolving conversation around homeopathy. Practitioners at all stages of their careers are warmly encouraged to register via the HINT website and take full advantage of this ongoing exchange.
HINT leads the way in promoting access to high quality research
Within this context, the role of professional organisations like Homeopathy International HINT becomes increasingly vital. HINT continues to lead the way in promoting access to high quality research while recognising that Homeopathy already has a three hundred and fifty year database of traditional usage, supporting practitioners with clinical resources, and engaging with healthcare systems on behalf of the profession. It plays a critical role in ensuring that studies like this one are not only read but understood, disseminated, and applied in meaningful ways.
The results of the Berrebi study also underscore the importance of being part of a professional body that champions our clinical experience through advocacy and evidence. As homeopaths, we often work in contexts that are under recognised or misunderstood by mainstream medicine. Having access to our copious materia medica and robust research, timely summaries, and a supportive professional network helps each of us practice with confidence and clarity.
Homeopathic principles translate into measurable outcomes
For students in particular, this study serves as an excellent example of how homeopathic principles translate into measurable outcomes. It’s a reminder that the art of remedy selection is not only clinically effective but increasingly defensible within the language of public health and evidence based medicine. Understanding such studies and being able to articulate their findings will be essential for the next generation of practitioners navigating a more integrative and interdisciplinary health landscape.
Ultimately, the study is a validation of what many of us have observed empirically: that homeopathy, when practised with care and skill, can make a profound difference in both acute and long term health. It also reflects a growing openness within the scientific and medical community to examine complementary approaches with intellectual honesty and methodological rigour. As this openness grows, so too does the need for homeopaths to engage, contribute, and advocate.